- Conditions
- Foot drop
Foot drop Paresis of the tibialis anterior muscle / paralysis of the tibialis anterior muscle
Introduction
Foot drop is a condition in which the foot can no longer be placed on the ground in a controlled manner when walking. The foot drops down, as it were, after the heel has made contact with the ground. Or the foot can no longer be raised at all and 'drags' on the ground. There is no longer any control because the muscles in the lower leg are weakened or failing completely due to a problem with the nerve.
Foot drop is also called paresis of the tibialis anterior muscle or paralysis of the tibialis anterior muscle.
Description of the condition
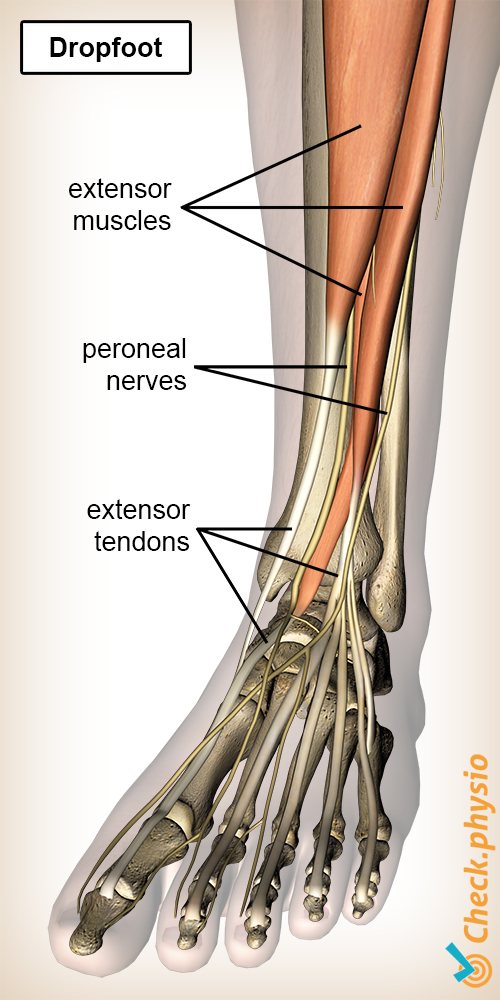
Foot drop is characterized by the loss of function of the muscles that lift up the foot, the so-called tibialis anterior muscles. Due to the fact that the tibialis anterior muscles have weakened, they can no longer control the heel-to-toe transition of the foot. Or the foot can no longer be lifted in its entirety so that the foot drags on the ground.
The muscles in charge of lifting the foot are:
- Tibialis anterior muscle.
- Extensor hallucis longus muscle.
- Extensor digitorum longus muscle.
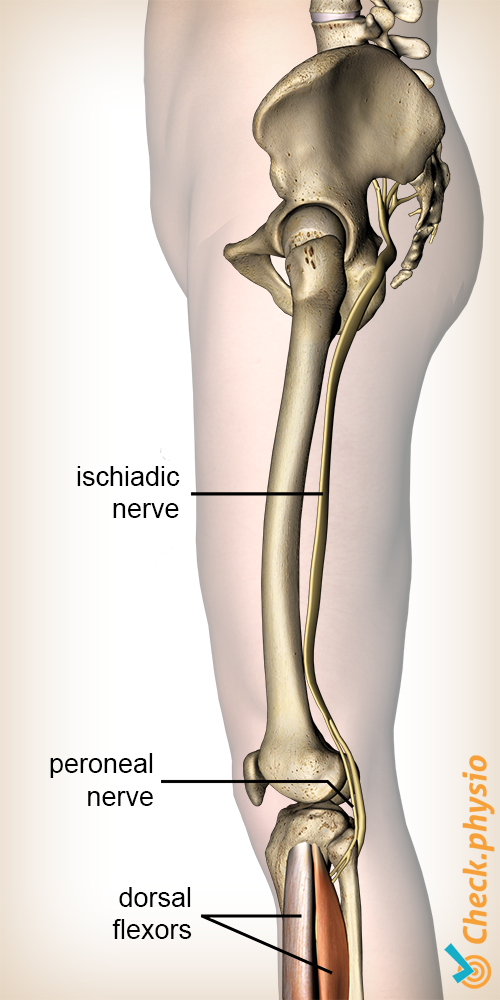
These muscles are controlled by the same nerve, the common peroneal nerve. When damage or entrapment occurs somewhere in the course of the nerve, there is a chance that the muscles no longer work properly.
Nerves originate in the bone marrow. The common peroneal nerve originates in the large leg nerve. This one is composed of nerves originating from the lower five vertebrae. The large leg nerve runs at the back of the hip, via the rear of the knee, towards the lower leg. The common peroneal nerve splits into two smaller branches in the lower leg.
Cause and origin
Pressure on the peroneal nerve can develop as a result of acute trauma, but a more gradual onset can also occur. Trauma can occur if the nerve is suddenly subjected to a lot of traction force, compression force or shift, such as in an hernia . Foot drop results from pressure on the nerve in the spine.
Signs & symptoms
A nerve entrapment usually follows a fixed pattern with clear characteristics of motor (muscle) and sensory (sensation) function loss.
In case of foot drop, the main symptoms are:
- Inability to lift the forefoot.
- No control or reduced strength of the muscles in the lower leg.
- Impaired walking pattern.
These are the symptoms that are immediately noticeable. In addition, there are other symptoms that can help determine where the nerve entrapment is located:
- Muscle weakness in the hip muscles.
- Muscle weakness in the knee flexors.
- Muscle weakness in the foot dorsiflexors.
- Muscle weakness in the toe extensors.
- Inability to walk on the heels.
In addition, sensory disturbances may be present when touching the skin. Or sensation may be completely absent in certain areas of the leg:
- Lateral side of the thigh.
- Lateral side of the lower leg.
- Top of the foot.
- Inner side of the foot.
- Between the first and second toe.
Diagnosis
The diagnosis of foot drop is usually easy to make, considering the changed gait pattern and the reduced strength of the tibialis anterior muscles. It is more difficult to find the cause of foot drop. This is due to the large overlap of complaints in the innervation area.
In order to gain proper insight into the problem, an interview is very important. Complaints such as back pain, the possible cause and the course of the complaints are important for a correct diagnosis.
Afterwards, a physical examination will be performed. This is to find out which muscles are weakened and where sensory changes occur. Also, reflexes will be tested in case foot drop is suspected with a cause coming from the spinal column.
When in doubt, or for verification purposes, the location of the entrapment can be examined with a EMG (nerve conduction test). If compression is suspected to be caused by a bone disorder or originates in the back, an MRI may be required to confirm this.
Treatment and recovery
The treatment is often conservative, i.e. without surgery. Only in case of compression due to bone disorders or other structural impingements, surgery can be a solution. The compression is then removed.
The physiotherapist often supports patients with these symptoms, although it is not usually necessary to see the physiotherapist frequently. Progress can be monitored well using targeted exercises and by regularly checking the muscle strength. Foot drop often recovers within a few months, but recovery can also take a year. If the physiotherapist does not see any progression in this period, or if it gets worse, further examination will be necessary. Besides physiotherapy, other possibilities include custom-made soles or a brace.
The treatment of foot drop that originates from the spine consists primarily of treating the spine.
Exercises
Take a look here at the exercise programme with exercises for drop foot.
More info
You can check your symptoms using the online physiotherapy check or make an appointment with a physiotherapy practice in your area.
References
Haveman, J.W. & Blomme, A.M. (2009) Beknelling van de N. peroneus superficialis. Een karakteristiek klachtenpatroon Ned. Tijdschr. Geneesk. 2009;153:B268; Isala klinieken, afd. Chirurgie, Zwolle.
Magee, D.J., Zachazewski, J.E., Quillen, W.S., Manske, R.C. (2016) Pathology and intervention in musculoskeletal rehabilitation Elsevier, 2nd edition.
Krishnamurthy, S. & Ibrahim, M. (2019) Tendon Transfers in Foot Drop Indian J Plast Surg. 2019 Jan; 52(1): 100–108.